Abstract
Introduction Novel agents including Bruton Tyrosine Kinase inhibitors (BTKi) have become the standard of care for patients with chronic lymphocytic leukemia (CLL). The ELEVATE-RR trial (NCT02477696) compared acalabrutinib to ibrutinib and demonstrated non-inferior progression-free survival (PFS) with fewer cardiovascular (CV) and bleeding adverse events for relapsed/refractory CLL patients treated with acalabrutinib (Byrd, et al. 2021). As baseline features and management strategies often differ between clinical practice and clinical trials, differences in outcomes may be observed. Thus, we conducted a real-world analysis of CLL patients treated with acalabrutinib vs. ibrutinib to compare outcomes in a non-trial population.
Methods This retrospective cohort study utilized electronic health record data from the Flatiron Health Database from July 2017 to February 2021. Patients with CLL or small lymphocytic lymphoma (SLL) were included if they initiated acalabrutinib or ibrutinib in any line of therapy (LOT) on or after January 1, 2018. Patients were followed to the earliest of last follow up or death with a data cut of February 28, 2021. Time to treatment discontinuation (TTD) was defined as the time from treatment initiation to discontinuation defined as start of a new LOT, lack of refilled prescription for ≥3 months, or death. Patients who did not discontinue BTKi treatment were censored at the last follow up.
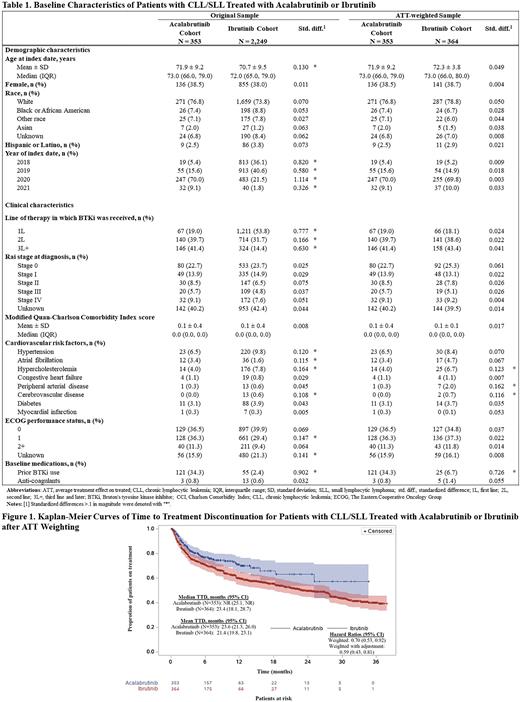
Average treatment effect among the treated (ATT) weighting was used to balance key baseline characteristics (age, sex, race, geographic region, year of index date, year of diagnosis with CLL or SLL, line of therapy, Rai stage, modified Quan-CCI score, atrial fibrillation, ECOG performance status, and use of anti-coagulants) and improve comparability between the cohorts. Kaplan-Meier analysis was used to estimate unweighted and weighted TTD. A weighted Cox proportional hazards (PH) model was used to compare TTD between acalabrutinib and ibrutinib.
Results From January 2018 through February 2021, 2,509 patients were identified and included in the analysis. Of these patients, 89.6% (n=2,249) received ibrutinib and 14.1% (n=353) received acalabrutinib across all lines of therapy. The acalabrutinib cohort had a median age of 73.0 years at drug initiation; the ibrutinib cohort had a median age of 72.0 years. Sex and race were similar in the two cohorts. After weighting to address significant differences across cohorts, the acalabrutinib cohort and the ibrutinib cohort were balanced on all baseline characteristics except CV risk factors (more common in the ibrutinib cohort) and prior BTKi use (more common in the acalabrutinib cohort; Table 1). Prior BTKi use was added as a covariate in the Cox PH model.
With a median follow up of 15.9 months for the entire cohort, TTD for acalabrutinib was significantly longer in weighted analysis of all patients compared to ibrutinib. The median unweighted TTD was not reached (NR) (95% CI: 25.1, NR) for the acalabrutinib cohort, whereas the median TTD was reached in the ibrutinib group (29.3 months; 27.7, 33.2). After weighting, the median TTD was still NR (25.1, NR) for the acalabrutinib cohort and was 23.4 months (18.1, 28.7) for the ibrutinib group (Figure 1). The discontinuation rate at 12 months was 22% for the weighted acalabrutinib cohort vs. 31% for the weighted ibrutinib cohort (p=0.005). After additional adjustments for prior BTKi use, the acalabrutinib cohort had a 41% lower risk of discontinuation vs. ibrutinib (HR 0.59; 0.43, 0.81; p=0.001) (Figure 1). Results stratified by LOT demonstrated a consistent trend toward superior TTD favoring acalabrutinib.
Conclusion We present the largest available experience comparing two BTKis, which demonstrates lower rates of discontinuation and a prolonged time to discontinuation for patients receiving acalabrutinib as compared to ibrutinib in both the front-line and relapsed/refractory settings. While randomized data have demonstrated similar PFS for patients treated with acalabrutinib and ibrutinib in the relapsed/refractory setting, these data provide valuable insight into how these agents compare in the front-line setting (not tested in ELEVATE-RR) and outcomes in clinical practice outside of the clinical trial setting. Data to be presented include reasons for discontinuation of each agent, additional follow up with a larger sample, and comparison based on available molecular genetic profiles.
Disclosures
Roeker:AbbVie: Consultancy, Divested equity in a private or publicly-traded company in the past 24 months; AstraZeneca: Consultancy; Beigene: Consultancy; Janssen: Consultancy; Loxo Oncology: Consultancy, Other: Travel support , Research Funding; Pharmacyclics: Consultancy; Pfizer: Consultancy, Research Funding; TG Therapeutics: Consultancy; Abbott Laboratories: Current equity holder in publicly-traded company; Aptose Biosciences: Research Funding; Ascentage: Consultancy; Qilu Puget Sound Biotherapeutics: Research Funding. DerSarkissian:Analysis Group: Current Employment; Takeda: Other: I am an employee of Analysis Group, Inc, which received research funding from Takeda for this study.; AstraZeneca: Research Funding. Ryan:AstraZeneca: Current Employment, Current equity holder in publicly-traded company. Chen:Analysis Group: Current Employment; AstraZeneca: Research Funding. Wahlstrom:AstraZeneca: Current Employment, Current equity holder in publicly-traded company, Divested equity in a private or publicly-traded company in the past 24 months. Hakre:AstraZeneca: Current Employment, Current equity holder in publicly-traded company, Divested equity in a private or publicly-traded company in the past 24 months. Yu:Analysis Group, Inc: Current Employment. Guo:AstraZeneca: Research Funding; Analysis Group, Inc: Current Employment. Mato:Genentech: Honoraria, Research Funding; BMS: Honoraria; Medscape: Honoraria; Nurix: Research Funding; LOXO: Honoraria, Research Funding; Curio: Honoraria; AstraZeneca: Honoraria, Research Funding; Pharmacyclics, LLC: Honoraria, Research Funding; PerView: Honoraria; Acerta: Research Funding; PER: Honoraria; BeiGene: Honoraria, Research Funding; Adaptive Biotechnologies: Honoraria; Genmab: Honoraria, Research Funding; Pfizer: Research Funding; DTRM Biopharma: Honoraria, Research Funding; AbbVie: Honoraria, Research Funding; Dava: Honoraria; Johnson & Johnson: Honoraria, Research Funding; Octopharma: Honoraria, Research Funding; TG Therapeutics, Inc: Honoraria, Research Funding; Janssen: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal